By Vicki Kaluza, Clinical Lead, Nervecentre Software
Three years ago, almost to the day, I wrote a piece about Sepsis to correlate with the release of the Nervecentre sepsis module. This time, on World Sepsis Day, I would like to look at where we are at with our success in this and Sepsis awareness in general.
A small recap- in 2015 I wrote…. “Sepsis can be severely debilitating or at worse fatal. It is also a condition that does not discriminate between age, gender or location. Whilst newborn babies, the elderly and those with compromised immune systems are the highest risk groups, sepsis can affect anyone of any sex and at any age, making it a condition that worldwide is a very real threat to anyone”. As true as this statement is this year I personally experienced how Sepsis can take someone who is fit and well at home and debilitate them for months. A close family member of mine collapsed at home with Sepsis and thanks to the extremely quick actions of the paramedic crew and the ED was treated promptly, but still endured an extensive hospital stay and gruelling 3-month recovery. This really drives home to me the importance of education and safety netting so none-of us lose someone because it ‘was missed’. The BBC documentary on this year that showed families having lost someone to sepsis was heart-breaking.
Are the numbers in general better or worse? …. Around 100,000 people in the UK every year are diagnosed with sepsis and around 37,000 people die as a result of the condition. According to the latest statistics, death rates attributed to sepsis are now 31,000 with 1,000 a year being children under 5 years old – all costing our NHS around £2 billion per year. So there appears to be some improvement but for something that is curable if treated quickly no-where near what we would like to see. Also, as coding improves year on year and the ability to determine cause of death is more accurate are the numbers changing or are the causes of death just more accurate? This could potentially appear to have a plato effect when in reality the numbers may be getting better but fewer deaths were correctly attributed to sepsis before.
Has awareness changed? … Yes, I believe with high profile media attention, with campaigns like world sepsis day, charity events and targeted information drives (the likes of which 3- 4 years ago we had only just begun to see), for sepsis has really brought more attention to both the clinical and non-clinical community. However, statistics show that in deprived areas this awareness and exposure to facts and media campaigns are not as successful and so we as a nation still have a long way to go before everyone understands Sepsis in the same way people understand what ‘Heart Disease’ or ‘Cancer’ is.
What level of response have NHS England given? …. The Sepsis CQUIN was introduced in 2015/16 and had some positive results in improving screen rates but in 2017 NHS England issued another 2 year CQUIN ‘Reducing the impact of serious infections (Antimicrobial 2. Resistance and Sepsis)’ directly aiming to encourage and challenge hospitals to improve performance on both identification and treatment of sepsis. Positive steps, but as 80% of Sepsis is not contracted within hospital it is critical that on admission to our hospitals immediate 100% screening is imperative. The introduction that a percentage of the CQUIN money is interdependent on the deployment of NEWS2 also shows the importance being placed on the detection of Sepsis with the introduction of a key indicator – Confusion/Delirium. Many Nervecentre NHS Trusts have been recording confusion as an indicator for several years within our observation module with tens of thousands of observations including this data prior to the RCP including this formally in the warning score. The transition ensures that across the country this indicator is considered every time. Nervecentre fully support NEWS2
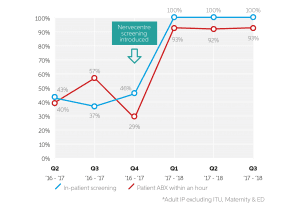
Nervecentre deployed our sepsis module with great success. At one of our Trusts, County Durham and Darlington NHS Foundation Trust, the success with this screening and reducing treatment times is exceptional. Prior to the introduction of Nervecentre screening, 46% of inpatients were screened for sepsis – with levels as low as 37% in Q3 2016/17. By May 2017, this had climbed to 100%. Similarly, the number of patients with sepsis receiving antibiotic treatment within one hour of diagnosis has risen significantly. Prior to the introduction of Nervecentre screening, the number of patients administered antibiotics within one hour of a sepsis diagnosis was 29%. In May 2017, that figured had grown to 93% – and has continued to perform in excess of 90% in the months that have followed.
In April 2018, Nottingham University Hospitals NHS Trust (NUH) completed a comparative analysis of its automated sepsis screening for adults. The analysis focused on a cohort of patients pre- and post- e-Screening, looking at the time to administration of first dose antibiotics. It showed a reduction of 20 minutes in median time to antibiotics across the trust. The reduction is more marked for inpatient areas (58 minutes) than for admission areas (3.5 minutes). The introduction of e-Screening has also reduced the variation in time to receiving treatment. NUH already had very successful screening rates due to the work they had implemented over the 5 years previous to deployment of sepsis e-screening with Nervecentre however the target was to improve further and this has been achieved.
With many more of our trusts currently having just deployed, or in the process of deploying the sepsis screening module we are confident that the screening figures will be 100% in our hospitals and the time to treatment radically improved. This will help save lives as well as trusts meet their CQUIN targets. We aim to help bring the death rate figures down year on year and have a world-class solution to support the NHS using our mobile-based tool that screens every single patient having observations entered (in real time) across our hospitals in ED, the admissions units, inpatient wards and Paediatrics.
About Vicki Kaluza: 14 years nursing experience both in the NHS and the RAF. A nursing background in Acute Admissions/Assessment Units and Coronary Care units across the country and with 4 years as a Hospital at Night Coordinator at Nottingham University Hospitals.
For the last 4 years work at Nervecentre as a ‘Clinical Lead’ supporting multiple trusts, product development as well as having a responsibility for Clinical safety.