NUH cuts discharge delays: the power of real-time data
Nottingham University Hospitals has more than halved the number of discharge-ready patients in its hospital beds – saving millions of pounds – thanks to real-time data enabled by Nervecentre.

Nottingham University Hospitals NHS Trust (NUH), and its partners in health and social care, worked with Nervecentre to create a digital solution that allows teams to track patients’ progress through complex discharge pathways, highlight bottlenecks, and drive accountability.
The solution is underpinned by a live dataset that’s updated dynamically by an integrated discharge team (IDT) spanning the whole care system (NUH, social care, community health). The IDT and executive teams access the data in real time, using it to guide and support system-wide decision-making.
The approach has significantly improved the timeliness of acute discharges out of NUH, helping to free up hospital beds, increase capacity for elective care, and ease the pressure on emergency pathways.
Here’s how it got there.
Discharge delays: a costly national problem
First, the bigger picture. Delayed discharges have long been a headache for NHS hospitals, wasting resources and blocking acute beds. Beyond financial implications – estimated to exceed £1.7 billion annually – the human costs, including patient deconditioning, are profound.
Most delays occur in ‘supported’ discharge pathways:
- Pathway 1: Home, with new or additional care needs
- Pathway 2: Care in an interim facility, often community bed-based settings, with dedicated recovery support
- Pathway 3: Long-term care in a nursing home or specialised facility
Delays in arranging care packages or finding suitable placements for patients on these pathways can result in extended hospital stays and significant downstream costs.
NUH, one of the busiest hospitals in England, was no stranger to the challenge. Pre-pandemic research showed that bed day losses caused by discharge delays were costing the trust around £20 million every year. Since then, NUH has been on a mission to fix it – and with the help of Nervecentre’s EPR, it’s made impressive strides.
The journey to reducing discharge delays
In 2023, NUH and its system partners began a workstream to enhance discharge functionality within its Nervecentre EPR. The goal was to build on its existing ability to identify discharge-ready patients by capturing additional information on why those patients were still in hospital beds. By achieving full visibility of system-wide delays and understanding their root causes, the team could align resources effectively, drive accountability, and end the blame culture.
Through whole-system engagement, Integrated Discharge Leads focused on understanding each organisation’s data needs, creating a list of common data requirements that could be captured via Nervecentre. These requirements provided the blueprint for development work to strengthen EPR functionality and inter-organisational interfaces.
A collaborative team from NUH, its system partners, and Nervecentre co-created and tested live dashboards that displayed where discharge delays were occurring and, crucially, why. These dashboards offered real-time insights into system bottlenecks, enabling organisations to visualise problems, address root causes, and mobilise resources.
One version of the truth
Today, teams across the ICS access a unified dataset – “one version of the truth” – via Nervecentre, working together to discharge patients back into the community. Live dashboards group discharge-ready patients by pathway, creating smaller, manageable cohorts. Previously, the IDT only saw total discharge-ready numbers, which often felt overwhelming. Now, each dashboard box represents a specific pathway with assigned team responsibility. With a single click, staff can identify and address pathway blocks, prompting swift action to resolve delays. This visibility drives accountability, expediting discharge processes.
The result? Discharge delays at NUH are trending downwards.

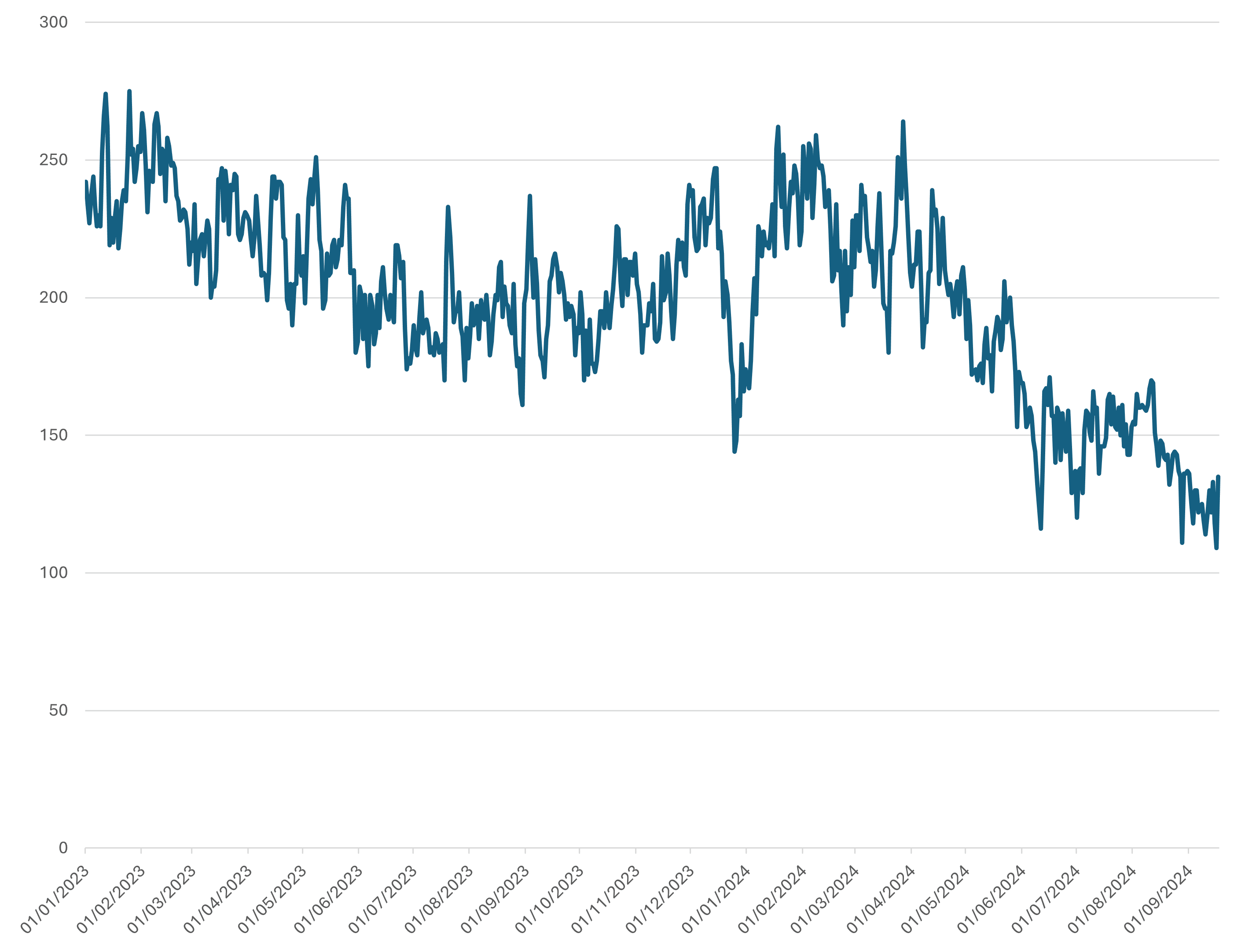
At midnight on 29th September 2022, 285 discharge-ready patients were stuck in NUH beds. Two years later there were 109 – a reduction of more than 60%.
Between April and December 2024, the number of discharge-ready patients in NUH beds overnight consistently hovered between 100-125, down from a winter-related high of 264 in March. In 2018/19, that number was routinely 250+.
The average post-medically safe length of stay has reduced by more than 3 days since 2017, meaning more beds are available to those who need them most.
Our experiences show that the issue of discharge delays – a seemingly intractable problem that the NHS has struggled with for years – is solvable. The solution comes from having a high quality, shared dataset, and tools that help teams action meaningful change. If you don’t have accurate data that’s visible to everyone in real time, you’ll fall short. But if you’ve got data you can trust, great things are possible. Five years ago, bed day losses were costing NUH around £20 million a year. Now, thanks to trusted, real-time data – and incredible collaboration across our ICS – we’ve halved those costs and have the latitude to go further. It shows that by being scrupulous around data – and having a fantastic system to record it on – you can get to a better place.
Marks Simmonds, Deputy Medical Director at NUH
Download the full case study
The PDF case study ‘From bottlenecks to breakthroughs’ contains more detail about how NUH is using data to help accelerate supported discharges.



